Abstract
Background: Allogeneic hematopoietic stem cell transplantation (HSCT) from an HLA-haploidentical relative (haplo-HSCT) is a suitable option for children/young adults with acute leukemia (AL) either relapsed or at high-risk of treatment failure and in urgent need of an allograft. A novel method of graft manipulation based on the selective, negative depletion of αβ T and B cells has been recently developed. We published the results of a prospective trial (ClinicalTrial.gov identifier: NCT01810120) enrolling 80 children with AL transplanted until September/2014 using this approach (Locatelli, Blood 2017). In the present analysis, we update those results, evaluating also additional patients given haplo-HSCT after that date.
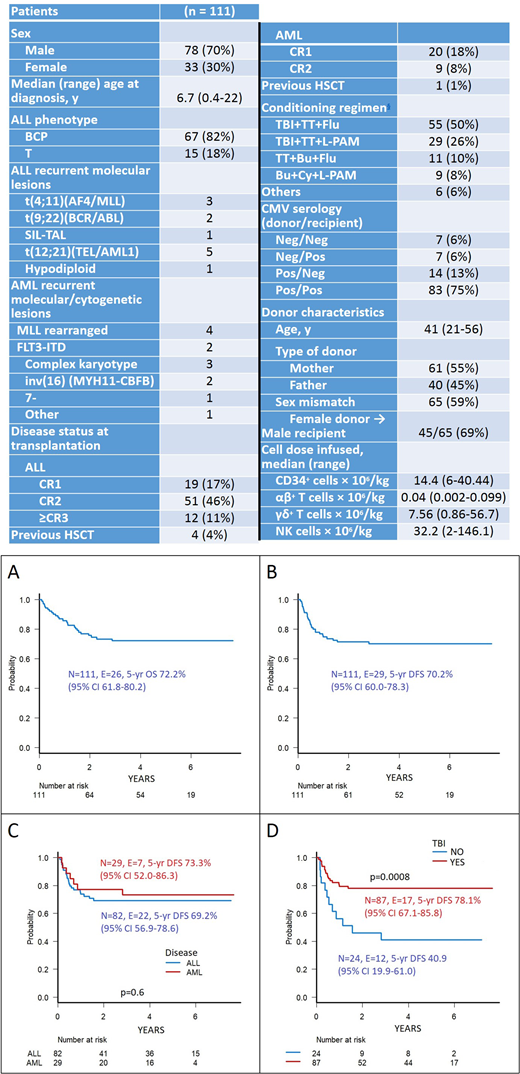
Patients and methods: Analyzed are 111 children with AL enrolled in the trial; median age is 10 years (range 0.9-22.2). Eighty-two (74%) and 29 (26%) patients had acute lymphoblastic leukemia (ALL) or acute myeloid leukemia (AML), respectively; they were transplanted between 09/2011 and 05/2018. All children were transplanted in complete morphological remission and received a fully myeloablative preparative regimen. Details on patients' characteristics, as well as on the number of HSC and lymphocyte subsets infused, are shown in Table 1. The donor was mainly chosen according to immunological criteria, giving priority to NK-cell alloreactivity, evaluated according to the killer immunoglobulin-like receptor (KIR)/KIR-Ligand mismatch in graft-versus-host direction model, KIR B haplotype, higher B-content score and size of NK alloreactive subset. Anti-T lymphocyte globulin (ATLG Grafalon®, Neovii Biotech) was administered at a dose of 12 mg/Kg from day -5 to -3 for preventing graft rejection and graft-versus-host disease (GvHD). Moreover, to reduce the risk of EBV-related post-transplant lymphoproliferative disorder (PTLD), on day -1, patients received rituximab (200 mg/m2) for in vivo depletion of both donor and recipient B cells. No patient was given any post-transplantation pharmacological GvHD prophylaxis.
Results: Median follow-up of surviving patients is 47 months (range: 2 months - 7.7 years). All patients but two successfully engrafted and the median time to neutrophil and platelet recovery was 13 (range 9-22) and 11 (range 8-20) days, respectively. Acute GvHD occurred in 28 patients; it was of grade I and grade II severity in 9 and 19 patients, respectively. Skin was the sole organ involved in all patients but one, who had gut involvement. The cumulative incidence of grade I-II acute GvHD was 25% (95% confidence interval, CI, 17-33). Four out of the 91 patients at risk developed chronic GvHD, in all cases of limited severity, the cumulative incidence of this complication being 5% (95% CI, 1-9). Six patients died for transplant-related complications, this resulting into a 5-year cumulative incidence of transplant-related mortality (TRM) of 6% (95% CI, 2-11). Twenty-three patients relapsed at a median time of 186 days (range 60-1012) after transplantation, the 5-year cumulative incidence of relapse being 24% (95% CI, 16-33). The 5-year probability of overall and leukemia free survival (LFS) were both above 70%, as shown in Figure 1A and 1B, respectively. The 5-year probability of LFS in children with ALL and AML was 69% (95% CI, 57-79) and 73% (95% CI, 52-86), respectively (Figure 1C). Use of total body irradiation (TBI) during the preparative regimen was associated with better patient's outcome (Figure 1D), since it protected against the risk of leukemia recurrence [18% (95% CI, 10-28) vs. 45% (95% CI, 22-66) in patients who did or did not receive TBI, respectively, p<0.01]. The correlation between use of TBI and better outcome remained significant in multivariable analysis, with a hazard ratio of 0.35 (95% CI, 0.16- 0.78, p=0.01) for LFS. The median CD3+ cell count on day +90, +180 and +360 were 247, 659 and 1380/mcl, respectively.
Conclusions: This study, reporting long-term outcome of a large population of children/young adults with AL, confirms that αβ T- and B-cell depleted haplo-HSCT is an effective option for patients in need of an urgent allograft and lacking an HLA-identical donor. While TRM is impressively low, the main cause of treatment failure is leukemia recurrence, whose incidence can be lowered by the use of TBI during the conditioning regimen. The remarkably low risk of chronic GvHD renders the approach attractive also in terms of patient's quality of life.
Locatelli:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Bellicum: Consultancy, Membership on an entity's Board of Directors or advisory committees; bluebird bio: Consultancy; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Miltenyi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal